All published articles of this journal are available on ScienceDirect.
Kinship and Containment: A Qualitative Study of Village Health Volunteers’ Roles in Community-Based COVID-19 Response in Thailand
Abstract
Introduction
The COVID-19 pandemic had profound effects globally, disrupting health systems, societies, and economies. This research explored the roles and experiences of village health Volunteers (VHVs) in managing COVID-19 at the community level.
Methods
A hermeneutic phenomenology approach was used to explore VHVs’ lived experiences and meaning-making in the community’s COVID-19 prevention. This method emphasized interpretation within cultural and social contexts. Forty VHVs from Health Region 8 participated as informants. We gathered data through focus groups and audio recordings, then used content analysis through an iterative process to identify key themes.
Results
COVID-19 control in Health Region 8 was driven by organically developed community mechanisms alongside formal support from public health authorities. VHVs, primarily middle-aged women, played a crucial role in surveillance, screening, and patient coordination within the community. The “spider web” network, rooted in kinship and rural social ties, effectively monitored mobility and mitigated transmission risks. This approach highlights the power of social and cultural capital in enabling effective community-based epidemic control.
Discussion
Community-driven efforts, led by VHVs and kinship-based networks in Health Region 8, played a vital role in COVID-19 control by complementing formal health systems. These findings highlight the importance of social capital and local knowledge, though regional focus and qualitative methods limit generalizability and call for further validation.
Conclusion
Leveraging VHVs and community networks enhances COVID-19 control by integrating social and cultural capital with formal health systems, advocating for inclusion of indigenous knowledge in epidemic preparedness to improve public health responsiveness and community empowerment.
1. INTRODUCTION
Coronavirus Disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is transmitted via droplets, direct contact with infected individuals, and airborne particles, resulting in widespread infections and deaths worldwide [1]. The World Health Organization declared COVID-19 a pandemic, emphasizing the need for airborne precautions. In response, the Thai government implemented public health measures and declared an emergency decree under the slogan “Stay at Home, Stop the Virus, for the Nation” starting on March 26, 2020 [2]. This included travel restrictions, curfews, and the closure of department stores, public spaces, and high-risk businesses to mitigate the spread of the virus [3-9].
These measures had profound direct and indirect impacts on various aspects of life, including the economy, society, public health, and individual livelihoods, resulting in widespread business closures [10-12]. Some industrial estates chose to cease operations entirely [13-15]. Employment was also heavily affected, prompting the implementation of strict outbreak management protocols at national, provincial, and community levels [16].
Public awareness of the severity of the outbreak increased as the number of infections and critically ill patients rose, overwhelming healthcare systems and resulting in shortages of hospital beds in urban areas [17]. This led to widespread job losses and a shift toward remote work, prompting a mass.exodus of workers from cities back to their rural hometowns, a phenomenon referred to as “the collapse of the bee nest” following the shutdown of businesses and the industrial sector [18].
This migration sparked fear, panic, and heightened vigilance among rural populations as they braced for the potential introduction of the virus into their communities [19-21].
A critical component of local disease control was the human-centered mechanism, particularly the role of VHVs, who undertook prevention, control, and health communication tasks to raise awareness among community members [22,23]. VHVs, primarily women, bore significant responsibilities during the pandemic. They acted as community health leaders, facilitators of participation, and communicators of health information, reinforcing public adherence to preventive measures during the first wave of the pandemic [24-26].
VHVs also contributed to fostering immunity awareness and community health resilience. In subsequent waves, their work was driven by a strong sense of volunteerism rooted in local kinship ties. This resulted in coordinated, compassionate efforts to monitor, support, and care for community members, as well as to detect changes that might indicate potential outbreak risks [27].
Within the cultural context of the Isan region, kinship networks were integral to daily life and traditions, such as Sum Saew communal gatherings involving shared meals, which, although posing risks for transmission, also facilitated communication and social cohesion [28,29]. These traditions, embedded in the normal rhythm of life, enabled VHVs to effectively manage the emergency, implement preventive measures, and promote disease control in their communities during the outbreak [30, 31].
The study of the roles of VHVs provides critical insights into the socio-cultural drivers that foster mutual support behaviors within communities. These include volunteerism rooted in a spirit of altruism and kinship-based relationships, which together constitute essential forms of social capital that enhance community resilience during times of crisis. Moreover, qualitative inquiry through a hermeneutic perspective reveals the meanings that community actors assign to their roles in safeguarding public health. This interpretive lens highlights how VHVs perceive their contributions, adapt to emerging challenges, engage in continuous learning, and innovate in response to local needs and circumstances.
These experiences offer valuable lessons for strengthening community capacity and resilience. They also provide a pathway for understanding the lived experiences of VHVs, gaining insights into diverse perspectives, and interpreting meanings through a hermeneutic lens [32-34]. Recognizing the individual experiences and interpretations of VHVs is crucial in health social science, as people assign meaning to events in unique ways. These insights are essential for developing effective models to enhance the capacities of VHVs and to inform guidelines for disease prevention and control at the community level [35,36].
2. MATERIALS AND METHODS
This study was based on hermeneutic phenomenology using qualitative research.
2.1. Participants
The study involved 40 VHVs residing in Health Region 8, selected through purposeful sampling with maximum variation to reflect diversity in age, experience, and geographical context. Participants were either recruited or broadly recommended by local health authorities based on their active roles in COVID-19 prevention and control, both prior to and during outbreaks in their communities.
Eligible VHVs were those recognized by fellow volunteers and community members for their contributions to the pandemic response and who were physically and mentally prepared for in-depth interviews. Suitability was jointly assessed by community health personnel and through the volunteers’ self-assessment and willingness to participate.
The selection process was supported by the local VHVs network and partner agencies, ensuring feasibility and relevance to the study context. The research team played a central role in final participant selection, guided by broad input from local health officials to ensure comprehensive representation of VHVs experiences.
Therefore, this research does not employ exclusion criteria, as the selection of key informants focuses on purposeful sampling to obtain in-depth and specific data regarding the phenomenon under study. The selection process for key informants follows rigorous procedures as previously outlined.
2.2. Study Area
Public health personnel at the provincial and district levels jointly selected the study communities, as described below. Purposive sampling was used for the study areas where COVID-19 protection and control operations were well carried out. This was considered alongside an R0 value that remained below 1, as well as the absence of reported COVID-19-related deaths in the area during the course of the outbreak. The study areas were selected based on specific characteristics, including border locations and high infection rates relative to population size, along with evidence of effective local operations. The selected communities included So Phisai District (Bueng Kan Province), Phon Phisai District (Nong Khai Province), That Phanom District (Nakhon Phanom Province), and Na Klang District (Nong Bua Lamphu Province).
2.3. Research Instrument
In this study, the researcher, a university lecturer and public health officer with expertise in qualitative research, served as the primary instrument for data collection through focus group discussions and audio recordings. The focus group discussion topics were reviewed by scholars and practitioners at the local level to ensure they aligned with the study’s objectives and secondary questions. This process facilitated informants in reflecting on their operational experiences, using a review technique employed by the research team to summarize, reflect, and invite volunteers to provide additional information. The questions were flexible, allowing informants to freely express themselves, share stories, life experiences, and perspectives on operations. The research team used the “Isan” dialect as the primary language to foster mutual understanding and establish a friendly relationship between the researcher and the informants [37].
2.4. Data Collection
Data collection, after obtaining approval from the Human Research Ethics Committee, was conducted during January and February 2022. The research team made an appointment with volunteers through a network of local health officials to conduct focus group discussions. After introducing themselves, the research team-built rapport with the VHVs to establish familiarity and trust. Subsequently, they clarified the objectives of the study and obtained informed consent from the participants. The focus group discussions were conducted at Subdistrict Health Promoting Hospitals (SHPHs) located in the designated study areas of each province, as previously mentioned, to ensure a private and familiar setting that fostered trust and openness among participants. In this study, a total of four focus group discussions were conducted (one session per group per province). Each session consisted of 10 VHVs who met the inclusion criteria and were selected to participate. The research team facilitated the discussions, which included obtaining consent for audio recording and conducting member checks during the sessions to ensure accurate interpretation.
Each focus group session lasted approximately three hours, allowing sufficient time to fully explore the discussion topics and facilitate participant exchange with data saturation.
A note-taker was responsible for creating a seating chart and documenting key points from the participants, including identifying speakers and summarizing their statements. During each discussion, two additional research team members served as assistants to support and ensure a smooth process. The audio recordings were later transcribed and cross-checked with the note-taker's records, and the accuracy of the information was verified together with local public health officers who work alongside VHVs in COVID-19 prevention and control. Support data analysis based on the phenomenological research approach designed for this study [38, 39].
2.5. Data Analysis
The data were immediately analyzed during the focus group discussions to generate follow-up or secondary questions. This analysis continued after the discussions between the research team and VHVs, comparing the data obtained from the field notes. The audio recordings from the focus group discussions were transcribed verbatim, capturing word-for-word details of the participants' responses, including local expressions, tone, and nuances.
The transcription process was followed by back-translation into Thai, conducted by a researcher who is a native of the Northeastern region (Isan) of Thailand. This researcher possesses a deep cultural and linguistic understanding of the Isan dialect, ensuring that the meanings and context embedded in local expressions are accurately interpreted and retained.
Subsequently, the researcher analyzed the completeness of the data from the transcription of the recordings using data tracing and iterative review techniques to ensure consistency and credibility. Data coding and analysis were conducted using ATLAS.ti software to assist in analyzing and categorizing themes. The thematic issues that emerged from the discussions were summarized and interpreted using the hermeneutic phenomenological approach as proposed by Max van Manen, which emphasizes the exploration of lived experiences through reflective, interpretive engagement with the data. [40].
3. RESULTS
3.1. Data on Area Context
Health Region 8 comprises seven provinces in the upper northeastern region, namely, Loei, Nong Bua Lam Phu, Udon Thani, Nong Khai, Bueng Kan, Nakhon Phanom, and Sakon Nakhon, shown in Fig. (1), with a population of about 5.6 million people in the responsible areas. Most of the population is aging and has moved to the industrial and tourism sectors in metropolitan areas. Most in the area were late working age, elderly, or students in the formal system. This is the key summary information of the provincial area in this study.
Bueng Kan, a newly established border province along the Mekong River, shares a boundary with the Lao People's Democratic Republic. Its predominantly rural economy is based on agriculture and interprovincial labor. The province benefits from strong community-based health systems, especially through well-trained VHVs. During the COVID-19 pandemic, Bueng Kan demonstrated an effective response through rapid community surveillance, the establishment of local screening checkpoints, and stringent border control measures. The implementation of home isolation in remote areas, in collaboration with local administrative organizations, exemplified an efficient community-based containment strategy.
Nakhon Phanom, characterized by its strategic location as a transnational corridor through the Third Thai–Lao Friendship Bridge, faced a high risk of disease importation due to cross-border mobility. The province capitalized on its “border health security” mechanism by integrating public health measures with the operations of security agencies. Surveillance and Rapid Response Teams (SRRTs) and VHVs played a critical role in proactive surveillance. The province also adopted digital tracking systems to monitor inbound travelers, enabling prompt and targeted interventions.
Nong Khai, a key economic gateway province, is marked by significant cultural diversity and high labor mobility, particularly within its special economic zone. Its COVID-19 response featured robust coordination through the Provincial Communicable Disease Control Committee (PCDC), which worked closely with local governments and military units. Proactive vaccination strategies were employed, including mobile vaccination units and community-based outreach programs, which effectively expanded vaccine coverage to marginalized and vulnerable populations.
Nong Bua Lamphu, a smaller, predominantly rural province, exhibited strong community cohesion and longstanding grassroots health networks. The local VHVs and women’s groups served as crucial agents in health communication and care provision during the pandemic. The province leveraged its social capital to implement culturally sensitive health education, volunteer support for home-quarantined individuals, and community-based care models. These efforts significantly reduced the burden on formal healthcare facilities and enhanced the resilience of the local health system.

Health Region 8 Map, Thailand.
3.1.1. Information on Key Informants
Of the 40 key informants, 32 were female. Most were aged over 40 years old and worked as VHVs for at least five years, and five VHVs still served in leadership roles. All participated in preventing and controlling COVID-19 in the community from implementing surveillance and prevention activities in the patient-free area until the present.
3.2. Mechanisms for Preventing and Controlling COVID-19 in the Community
The prevention and control of COVID-19 by VHVs required cooperation from agencies and personnel in both the public and private sectors. As frontline workers in the community, VHVs received support from public health agencies and personnel in terms of knowledge and operational skills, including control, supervision, and follow-up, to effectively implement surveillance and prevention activities. As mentioned, “We worked closely with local health officers and received regular updates on how to manage suspected cases. The support helped us feel confident to monitor and protect our communities.” (VHVs,Bueng Kan)
The role of caretaker for disease prevention in the community was assigned to VHVs during periods with no outbreak. They were responsible for the surveillance of risk groups and monitoring the movement of people in the area. This included a mechanism and system for reporting, detecting, and assessing the risk of outsiders entering the area through history taking and referrals to public health and administrative agencies, as illustrated in Fig. (2). Additionally, they played a role in collaborating with the community to manage and provide quarantine spaces for relatives or community members who needed to return home during the severe epidemic in the industrial area, referred to as “The collapse of the bee nest” (VHVs, Nakhon Phanom). As mentioned, “When there were no confirmed cases in the village yet, we had to monitor entry and exit points every day, checking who was returning from other provinces or factories. We conducted interviews and immediately reported to public health officers. We were the first line of defense to prevent the virus from entering the community.” (VHVs Bueng Kan)
“Our role was not just taking temperatures or handing out masks. We had to assess the risk of incoming individuals and forward the information to the public health team right away. It was about working as one team with the whole village.” (VHVs Nakhon Phanom, Nong Bua Lamphu)
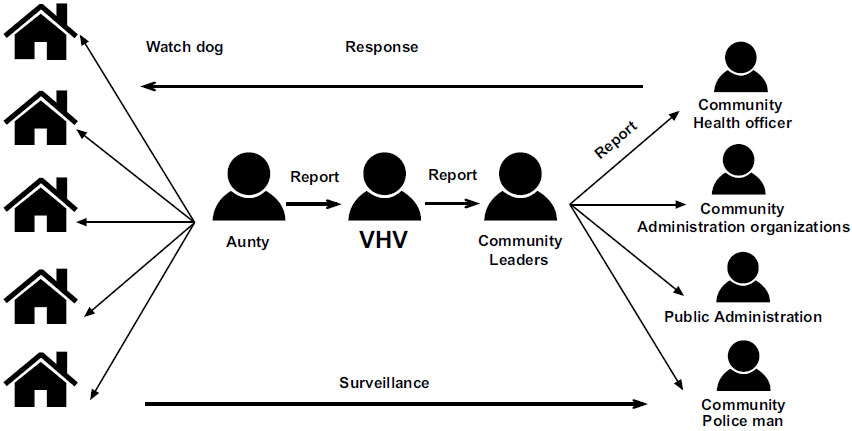
Regarding surveillance during the severe outbreak in both urban and rural areas, one of the key mechanisms for prevention and monitoring within the community was neighbors, referred to by teenagers as “Aunty Next Door.” This term was used to describe volunteers and middle-aged women who tracked the movements of adolescents and other community members. Motivated by fear, concern, and worry for the health of their families and community, this natural mechanism served as an important tool for disease surveillance by monitoring population movements within the community. Consequently, any suspicious activities were promptly reported to community leaders and volunteers, as previously mentioned. “They call us ‘aunties next door’ because we know who goes where and when—especially when teenagers or factory workers come back from the cities. We keep an eye on whether they’ve quarantined, and sometimes we have to call the village head or the health center. We do it because we care about the health of everyone, like they’re our own children.” (VHVs Nakhon Phanom, Bueng Kan)
The role of coordinator and facilitator in disease control with patients in the community was a joint operation with agencies and personnel from local administration organizations in infection control, patient referral management, quarantine, and community isolation. However, based on the situation, the operationalroles changed according to the context and characteristics of work. As for work during the outbreak and isolation of patients, the VHVs adapted themselves to support and facilitate the isolated patients and acted as a coordinator with the community, including the supply and allocation of essential items needed in life for patients and risk groups. As mentioned, “When people started coming back from industrial zones, we had to find quarantine sites ourselves. We worked with the village headman, local authorities, and the community to set up local quarantine facilities because we knew that without them, the whole village would be at high risk.” (VHVS Nong Bua Lamphu, Nhong Khai).
Most volunteers were “females” caring for people's health with a focus on illness and recovery of family and community members as the original capital. As a result, mechanisms for disease prevention and control in the community were well enhanced. The seriousness of their duties for disease prevention and control became a mockery among Isan teenagers, as “Aunty Next Door” detects every movement of people in the community as well as people outside the community to keep the community safe from the COVID-19 pandemic. As mentioned, “Once we heard that infections were rising in the cities, we became more vigilant. Wherever we went, there were always people helping watch out—looking for new faces or outsiders in the village. People did it out of fear, yes, but also out of love for their families and community.” (VHVs)
Hence, mechanisms for COVID-19 surveillance in Isan communities were naturally driven by fear and anxiety. Surveillance and detection of people’s movements in and out of the community aimed to identify the risk of the disease entering the area. In the context of rural society in the northeastern region, people live in groups based on kinship ties and the presence of elderly family members. Movements of individuals in and out of the community could be observed or perceived by community members. Additionally, during the COVID-19 outbreak, government measures were implemented to control and limit people’s movement to reduce the spread of the disease.
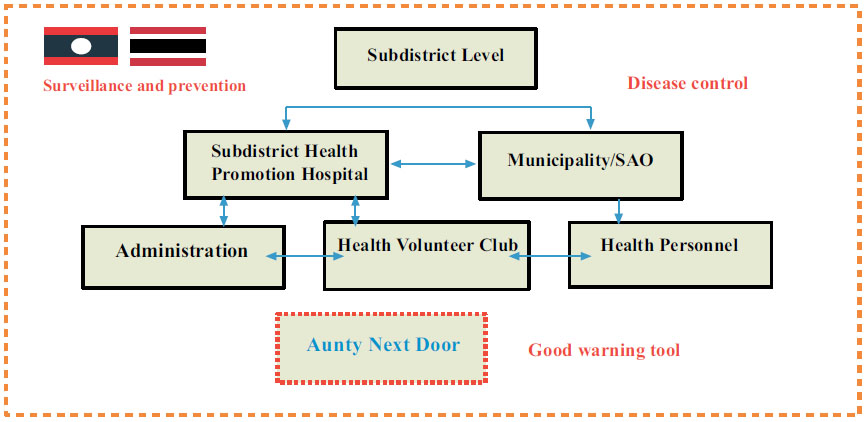
Mechanisms for preventing and controlling COVID-19 in the community.
Therefore, detecting the movement of people within the community was one of the measures used as a guideline for monitoring the risk posed by individuals traveling from one area to another, especially those coming from outbreak zones into communities where no COVID-19 cases had been reported. As mentioned, “Sometimes we didn’t even need to walk door to door. Neighborhood aunties, the ones who usually sit out in front of their houses, would notice any unfamiliar faces or young people coming back from elsewhere. As soon as they saw something unusual, they’d come tell us right away. We call it “community surveillance by watchful eyes.” (VHVs Bueng Khan)
Such mechanisms detected community movements through a group of “women” who prioritized illness and health for both themselves and their family members. These mechanisms naturally developed alongside public sector surveillance systems, which required reporting the entry and exit of people in the community. Systematic risk screening was conducted by monitoring the movement of “strangers” entering the community during an outbreak. Suspicious activities were reported to VHVs and community leaders to implement surveillance and disease control measures. According to local protocols, strangers were quarantined separately following community guidelines. The mechanism for detecting such movements functioned like a spider web, involving the joint efforts of “Aunty Next Door,” who monitored suspicious movements around their own homes. Public Health Volunteers relayed information and carried out surveillance, screening, and disease control management in the community according to public sector guidelines, covering eight to ten households. Community leaders managed surveillance and disease control by coordinating prevention and control efforts within their communities, working together with VHVs, public health officers, local administrative organizations, and public agencies. This spider web-like system is illustrated in Fig. (3).
From Fig. (3), the disease control mechanisms in the community can be divided into two phases, as detailed below:
Phase 1: Naturally developed mechanisms for disease surveillance involved monitoring the movement of people entering and leaving the community during the outbreak by women housekeepers. They reported suspicious activities to VHVs, who then reported these movements and proceeded with screening, surveillance, and disease control in collaboration with community leaders, public health officials, and local government officers.
Phase 2: Disease control mechanisms involved the active participation of VHVs, community leaders, public health officials, and local government officers in risk screening. This included temperature measurements, checking travel histories, community isolation, waste management, providing food for people in quarantine, and assigning guards to support isolated patients. The process also involved security and police officers playing a role in law enforcement to control isolated patients who violated laws and community rules, serving as advanced social measures for disease control during the outbreak.
Public sector's surveillance mechanisms.
4. DISCUSSION
This study illuminates the phenomenon of COVID-19 prevention and control in rural northeastern Thailand, with a focus on the roles and functions of VHVs through a phenomenological and socio-health analytical lens. The findings reflect not only the structural functions of VHVs but also the community's informal social mechanisms that emerged in response to the pandemic crisis.
The government’s measures for disease control were implemented at the area level, establishing a standardized mechanism under the provincial communicable disease prevention and control committee. This represented an integrated effort involving multiple sectors to address problems and operate at the community level, utilizing guidelines and applying social capital specific to each area for effective management. At the community level, disease prevention and control combined the guidelines set by the public sector with community-based mechanisms. Women, community health leaders, and VHVs played a crucial role in driving these efforts within local community health.
VHVs as frontline agents of the state: The role of VHVs during the COVID-19 outbreak involved proactive operations and integration with public health units and local administrative organizations. At the early stage of the pandemic, VHVs received knowledge and skills training from state agencies and played a crucial role in disease surveillance and systematic reporting [41]. This aligns with the public health paradigm that “health is everyone’s responsibility” and that health is a “social phenomenon” [42], which emphasizes that disease prevention cannot rely solely on medical professionals but must engage the community as co-actors in health governance.
Informal surveillance through local cultural mechanisms: a particularly noteworthy finding was the role of the “auntie next door” as a natural surveillance mechanism, reflecting the kinship-based and proximity-driven social structure of rural communities. Middle-aged women, often the caretakers of their households, assumed informal roles in monitoring unfamiliar individuals entering the village. This practice emerged as a form of social surveillance, rooted in cultural capital and social capital [43], demonstrating the power of local social practices embedded within the community. Such mechanisms are shaped by the lived experience of fear and anxiety, which were reinterpreted and restructured into meaningful community actions. These women did not act out of obligation alone but from a shared understanding of the risk posed by the disease to themselves and others [44].
Localized health governance and network coordination: the collaboration among VHVs, village leaders, state officers, and security personnel represented a form of place-based health governance that emerged during the pandemic crisis. This system involved network-based coordination not solely directed top-down by the state, but also through bottom-up mechanisms driven by community ownership and shared ethics [45 ]. This phenomenon reflects the concept of “Social Determinants of Health” highlighting that community health outcomes are not determined solely by medical services but also by sociocultural context and the community’s capacity to control local health resources [46].
VHVs and the role of grassroots women in health promotion: Most VHVs are women who have historically been viewed as “invisible labor” within the health system. However, during this crisis, their roles became pronounced as frontline caregivers who bridged personal, social, and state health systems. This aligns with Cornwall’s [ 47] notion of “gendered citizenship,” where women’s leadership in health and community life becomes central, particularly in times of crisis.
5. LIMITATIONS
This study, conducted in a single health region using purposive sampling, may have limited generalizability of its findings. Group dynamics within focus group discussions could have shaped participant responses. The exclusion of perspectives from community members and other stakeholders may have limited the depth and diversity of insights. Moreover, the evolving nature of the COVID-19 pandemic may influence the long-term relevance of the results.
CONCLUSION
This study reveals that the success of COVID-19 prevention in rural northeastern Thailand was not solely the result of formal health interventions but was deeply rooted in the synergy between state-mandated roles and informal community-based mechanisms. VHVs played a pivotal role in bridging government health directives with local values, while informal actors, particularly middle-aged women, functioned as culturally embedded surveillance agents. These findings underscore the importance of recognizing local knowledge and social capital in public health strategies. Future health policies should institutionalize community-led surveillance and strengthen gender-sensitive support for VHVs. However, the study is limited by its regional focus and reliance on qualitative data from a single cultural context. Further research should explore comparative models across diverse communities and examine the sustainability of such mechanisms beyond crisis periods.
AUTHORS' CONTRIBUTIONS
The authors confirm contribution to the paper as follows: W.N.A, R.K., L.W., and S.C.: Study conception and design; W.N.A, L.W., T.S., S.K., and S.C.: Data collection; W.N.A, L.W., and S.C.: Analysis and interpretation of results; W.N.A, L.W., and S.C.: Draft manuscript; All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease 2019 |
| SARS-CoV-2 | = Severe Acute Respiratory Syndrome Coronavirus 2 |
| VHVs | = Village Health Volunteers |
| SHPHs | = Subdistrict Health Promoting Hospitals |
| SRRTs | = Surveillance and Rapid Response Teams |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee, Institute for the Development of Human Research Protections (IHRP), COA NO. IHRP2021076 IHRP No.027-2564.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from each participant before participating in the study.
AVAILABILITY OF DATA AND MATERIALS
The data sets used and/or analysed during this study are available from the corresponding author [S.C.] upon request.
FUNDING
This research work was supported by Thailand Science Research and Innovation under the project “Lesson Learnt on public health emergency management of COVID-19 in many provinces nationwide” (Grant number: 63564).
ACKNOWLEDGEMENTS
The researchers would like to express their sincere gratitude to all the VHVs in Health Region 8 for their cooperation and time dedicated to participating in this study. We also extend our thanks to community leaders and public health officials for their support in providing information and facilitating operations. Additionally, we acknowledge the contributions of public health agencies and local organizations that assisted in data collection, as well as the experts who offered valuable insights for the development of this research. Finally, we thank everyone who contributed to the success of this study.


