All published articles of this journal are available on ScienceDirect.
When Bilateral Mastitis is not Mastitis: Primary Breast Burkitt Lymphoma in Pregnancy - A Case Report and Literature Review
Abstract
Background
Primary breast Burkitt lymphoma (PB-BL) is a rare, aggressive, malignant tumor of the breast that affects women of reproductive age during pregnancy or lactation. It can mimic benign and inflammatory conditions, leading to delayed diagnosis that inversely affects the prognosis. Here, we present a case of lactating women with no identifiable risk factors who were misdiagnosed as inflammatory mastitis, delaying the diagnosis to the postpartum period.
Case Presentation
A 32-year-old female in her third trimester of pregnancy presented with progressive bilateral breast enlargement and was initially mismanaged as inflammatory mastitis that failed to respond to multiple courses of antibiotic therapy. Following the delivery, as the woman continued to suffer with no improvement, the imaging study and mammography showed multiple matted heterogeneous, hypoechoic masses with increased vascularity and bilateral massive breast-positive axillary lymph nodes consistent with BIRAD-4c, suggesting malignancy. Multiple breast biopsies were taken with fine needle aspiration of the lymph nodes. Histopathology and immunohistochemistry revealed a starry sky morphology with Ki-67 proliferation, c-MYC overexpression, and CD10 positivity, confirming the diagnosis of primary breast B-cell lymphoma of the non-Hodgkin type. Intensive chemotherapy was started with follow-up.
Conclusion
The physician should practice a high index of suspicion when a breast condition presents with an aggressive course or when it fails to respond to medical therapy, even in the absence of risk factors. Imaging can help exclude potential diagnoses, but the gold standard remains histopathology and immunohistochemistry. The current case emphasizes the importance of early diagnosis and timely intervention, which are positively associated with improved patient survival.
1. INTRODUCTION
Primary breast Burkitt lymphoma (PB-BL) is rare; it accounts for 0.04-0.5% of all breast malignancies and represents 1.7-2.2% of all extra-nodal lymphomas. Primary breast lymphoma is classified based on the cell type and the clinical presentation (Fig. 1) [1]. According to the histopathological classification based on cell type, T-cell lymphoma is rare and typically arises near the site of a breast implant. The more common type is B-cell lymphoma, which accounts for approximately 90% of all cases [2].
The most frequent variant of B-cell lymphoma is diffuse large B-cell lymphoma, seen in 90% of cases, while Burkitt lymphoma is rare. This classification helps determine the aggressiveness of the lymphoma and aids in choosing the treatment plan. For example, fast-growing types, such as Burkitt lymphoma, require urgent treatment to improve patient prognosis [3].
The other classification is the clinical classification and laterality of the lesion presented; it can be bilateral, diffuse, or unilateral. The bilateral type is typically observed in younger patients and is often associated with pregnancy and postpartum. It is aggressive and tends to metastasize into the brain and ovaries, yet it typically spares lymph nodes (LN) [4]. As for the unilateral type, it affects older cases and tends to be localized to one side. It demonstrates lower metastatic potential, reduced aggression, and a good response to treatment [5].
This classification predicts the disease behavior and guides a tailored therapeutic approach based on the expected course of the disease.
1.1. Risk Factors for PB-BL
Many risk factors have been linked to an increased risk of PB-BL. These include demographic factors, socioeconomic hormonal factors, infections, and lactations, as summarized in Table 1.
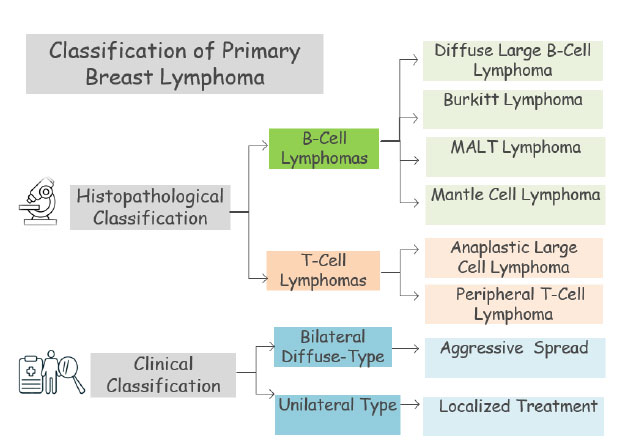
The classification of primary breast lymphoma.
| Parameter | Description | Associated Risk | References |
|---|---|---|---|
| Demographics | Age | • It affects adolescents and women of reproductive age (range 12-36 years) • Individuals of older age can be affected too |
[6] |
| Gender | Females are primarily affected, but it is reported in males | [7] | |
| Geographical | Globally reported, but some African regions are endemic | [8] | |
| Lower socioeconomic | Particularly common among endemic areas | [9] | |
| Hormonal factors | • Pregnancy, puerperium, and lactation • Hormonal changes |
• Those diagnosed during pregnancy tend to be bilateral • There was a report of an affected male while he was on anti-androgen therapy (spironolactone) for a malignant condition |
[6] |
| • Infections and immunocompromised patients |
Epstein-Barr virus | It is considered a key player, especially in endemic areas | [10] |
| HIV/AIDS | Strongly contribute to a reduced immunity state predisposing to PB-BL | [5] | |
| Malaria | It is considered a key player, especially in endemic areas | [9] | |
| Hepatitis C virus | Risk factors, especially for older adults | [11] | |
| Breastfeeding and maternal stress | Indirect effect | • Breastfeeding reduces a child's risk of childhood blood malignancy by 20% • Maternal stress may trigger immune dysregulation, increasing viral infection risk, such as EBV or reactivation of latent infection. Additionally, there is the risk of stress-related inflammation |
[12] |
The affected cases typically present with an aggressive course, characterized by bilateral rapidly enlarging breast masses, accompanied by erythema, systemic symptoms, and, in some cases, axillary lymphadenopathy. The diagnosis relies on imaging studies and is confirmed by histopathology and immunohistochemical analysis [4].
In imaging studies, PB-BL typically shows as unilateral or bilateral multifocal breast masses exceeding 5 cm in diameter, sometimes involving the entire breast. The masses have indistinct margins with thin skin, oedema of the subcutaneous region, and echo enhancement. On ultrasound, the masses are hypoechoic, surrounded by a hyperechoic area having a reticular structure. There is enhanced vascularity and abundant internal and peripheral blood flow; calcification is rarely seen [13].
Histologically, PB-BL exhibits diffuse lymphoid cell infiltration and hypoechoic nodules with reticular fibrous structures. Microscopically, the tumors have a characteristic “starry sky” appearance, resulting from high proliferation and extensive apoptosis rate among lymphoma cells.
2. CASE PRESENTATION
A 32-year-old female G2P2A1, with both deliveries involving a C-section, presented with progressive, painless breast enlargement. The condition initially started in the 26th week of pregnancy when she noted a gradual increase in breast size, engorgement, and heaviness with pigmentation changes. She denied having nipple discharge or skin changes. The symptoms were more pronounced on the left side of the breast. Despite seeking advice at multiple clinics, she was reassured that the symptoms were related to hormonal changes in pregnancy. However, after giving birth, her symptoms became significantly worse. She had rapid, painful breast enlargement, accompanied by a low-grade fever persisting for 4 months postpartum.
2.1. Physical Examination
Upon examination, both breasts were enlarged, with the left breast being more prominently affected. They appeared engorged and erythematous with multiple palpable, hard, matted masses. The skin exhibited pigmentation, swelling, and engorgement of the superficial veins; however, there were no nipple changes, discharge, or Peau d’orange appearance (Fig. 2). Additionally, bilateral palpable axillary lymphadenopathy was noted. Other LN examinations were negative, including supraclavicular, groin, neck, and pre- and post-auricular regions.
After multiple consultations with various physicians and receiving treatment for acute inflammatory mastitis with multiple courses of antibiotics, the patient showed no improvement. She presented to our clinic for further evaluation. After physical examination, a mammography and ultrasound examination of both breasts, alongside the axilla and the abdomen, were performed.

Physical examination showed hard matted masses, pigmentation, and swelling, as well as redness with engorgement of superficial veins, in addition to bilateral palpable axillary lymphadenopathy.
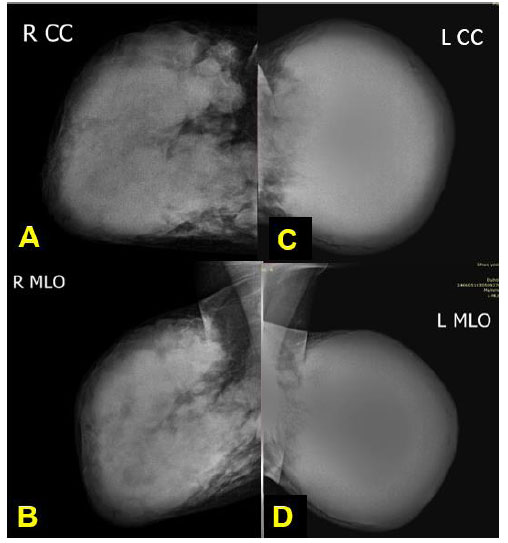
Mammography: CC and MLO (A, B) views of both breasts show extremely dense fibro glandular tissue with multiple different sizes of hyper-dense obscured margin matted masses at the right breast region. (C) The left breast shows a large, ill-defined block of hyper-dense mass that was very firm at the examination and even was non-compressible during the mammographic procedure; no visible normal fatty tissue, no associated microcalcification, and no nipple abnormalities were seen. (C,D) Bilateral axillary lymph nodes were noted to be round to oval in shape with loss of fatty hilum, categorized as BIRADS 4c.
The mammography (Fig. 3A-D) and ultrasound examination (Figs. 4A-C, 5A-B) showed BI-RADS 5. It was very suspicious of an aggressive malignant process, given the identification of multiple matted masses with increased vascularity and bilateral lymphadenopathy. In light of these findings, multiple core needle biopsies from both breasts and fine needle cytology from the axillary LN were strongly recommended to confirm the diagnosis. Figs. (6A-D and 7A-D) highlight histopathological findings.
At this point, the differential diagnoses included the following:
- Chronic mastitis, idiopathic or granulomatous mastitis
- Pregnancy-associated breast cancer
- Inflammatory breast cancer
- Phyllodes breast tumor
- Lymphoma, whether primary Burkitt lymphoma of the breast or metastatic lymphoma arising from a systemic non-Hodgkin lymphoma.
- Other hematological malignancies, including leukemic infiltration.
Based on imaging, histopathology, and immunohistochemistry results, the breast's primary Burkitt lymphoma (PBL) was confirmed. Then, the patient subsequently underwent a total body scan, PET-CT scan, and hematologic oncology work-up, confirming stage III disease.
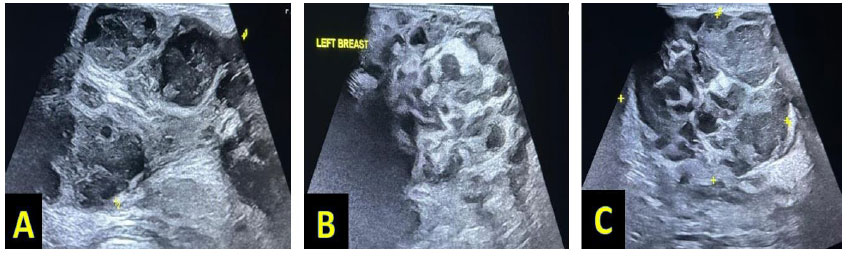
(A) Right breast showed a loss of normal breast tissue architecture with multiple partially circumscribed round-shaped heterogenous masses, mainly hypoechoic in texture and at subareolar region extending into axillary tail region, seen matted together forming large masses, with the largest one measuring about 7x 4, 5x 3.7 cm, showing posterior enhancement, with peripheral and internal few vascularities, and the masses being suspicious of malignancy, categorized as BIRADS 4c. (B,C) Left breast showed loss of normal breast tissue architecture replaced by multiple round to oval-shaped partially circumscribed heterogeneous masses, being mainly hypoechoic in texture and matted together, with the largest ones measuring about 10x 6, 8x 4 cm, showing posterior enhancement with few peripheral and internal vascularities, and involving the whole breast tissue region, thus causing mass effect at superficial veins and subcutaneous tissue. The masses were similar to the right breast masses, but larger in size, suspicious of underlying malignancy, and categorized as BIRADS 4c.
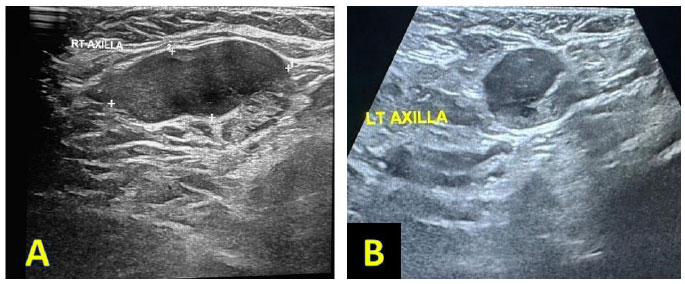
Ultrasound examination of the right (A) and left (B) axillary regions showed enlarged axillary LN being round to oval in shape; most of it showed efface distorted hilum, thick cortex being about 7-8 mm in size, with the largest one measuring about 24x17 mm, 21 x 16 mm. All of these findings were suspicious of pathological LN and fine needle aspiration (FNA) from both axillary regions.
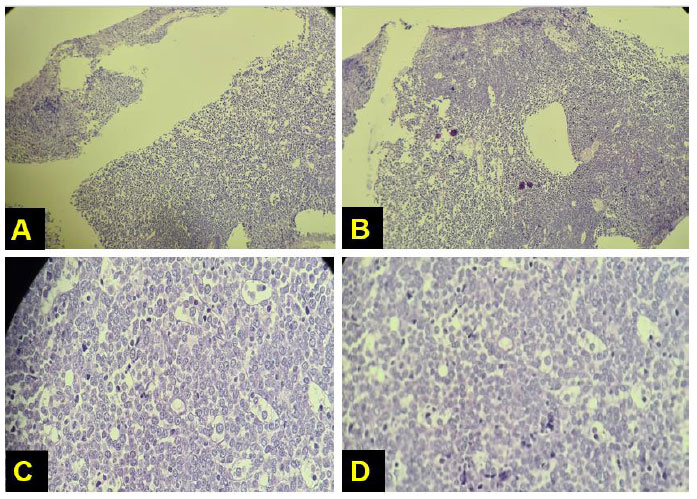
(A, B) True cut biopsy of breast (low power; X20) showed diffuse proliferation of intermediate-sized atypical lymphocytes with a focal starry sky appearance. (C, D) True cut biopsy of the breast (high power, X 40) showing diffuse proliferation of intermediate-sized atypical lymphocytes with a focal starry sky appearance.
All investigation results and workflow are summarized in Table 2. The patient received four courses of chemotherapy, including the R-HCVAD regimen, comprising rituximab, cyclophosphamide, doxorubicin (adriamycin), vincristine, and dexamethasone, as well as intrathecal chemotherapy for neuroprophylaxis, such as cytarabine. Supportive medication was given to mitigate drug toxicity, represented by folinic acid. The lesions significantly regressed, and the breast region had a normal appearance. The patient has been in remission since then and continues to follow up with an oncologist on a monthly basis.
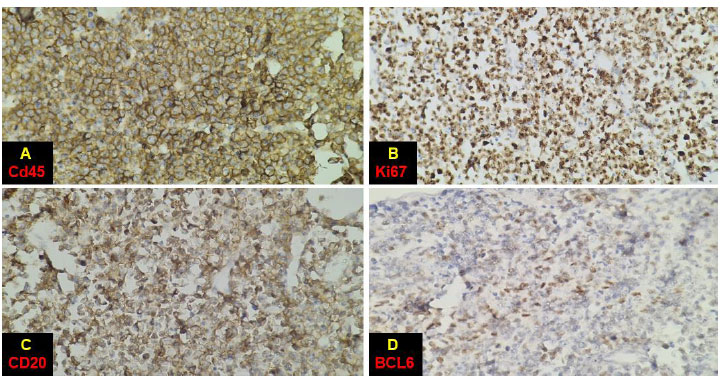
Breast histopathological slides. (A) Diffuse expression of CD45; (B) Ki67 was positive in more than 90% of cells; (C) diffuse expression of CD20 (B-cell marker); (D) expression of BCL6 (germinal center marker) in 50% of cells.
| Intervention | Results |
|---|---|
| Mammography | Both breasts showed extremely dense fibro-glandular tissues, limiting radiological sensitivity. No microcalcifications nor nipple architectural defects were detected. • Right breast: Multiple hyperdense, matted masses of varying size were identified with indistinct margins, raising malignancy suspicion. • Left breast: A large ill-defined, hyperdense mass was observed in a single solid block that was very firm and non-compressible at mammogram examination, during compression, categorized as BIRADS 4c. • Axillary finding: Bilateral axillary lymphadenopathy was noted (Figure 2). |
| Breast ultrasound | The typical breast architecture was lost and replaced by multiple heterogeneous, predominantly hypoechoic masses that appeared matted together, making it hard to discriminate them individually. These masses showed internal and peripheral vascularity, suggesting increased perfusion. • Right breast: the largest mass measured 7×4× and 5×3.7 cm. • Left breast: the largest mass measured 10 ×6× 8× 4 cm. • Axillary finding: Bilateral enlarged axillary LN with distorted hilum and thickened cortex, raising suspicion of metastasis. The largest one measured about 2x1.7 cm (Figure 3C, D). Categorized as BI-RADS-4c: It was highly suggestive of malignancy; thus, a biopsy was strongly recommended. |
| Multiple core needle biopsies on both breast masses and fine needle biopsy (FNB) on axillary LN |
The histopathology report showed a diffuse proliferation of atypical, intermediate-sized lymphoid cells infiltrating the terminal duct-lobular units, exhibiting a characteristic “starry sky” morphology. |
| Immunohistochemistry findings showed the neoplastic cells to be as follows: • Positive for CD20, CD10, BCL6, and CD45 • Negative for CD3, cyclin D1, BCL1, and CD23 • The proliferation index (Ki67) being 100% • High expression of c-MYC Final diagnosis: The features were consistent with bilateral breast Burkitt lymphoma (BL). |
|
| Hematologic oncology ward work-up | • Complete blood count (CBC) • Bone marrow aspiration • Cerebrospinal fluid analysis (CSF examination) All were within normal ranges, and no involvement was detected |
| Body scan study | • Chest X-ray • Abdominal ultrasound scan Both showed no abnormalities • A PET CT scan showed stage-3 disease. |
| Patient age (years) | Gestational age at diagnosis | Delivery mode | Maternal outcome | References |
|---|---|---|---|---|
| 40 | 27 weeks | C- section | Alive | Cordeiro et al., 2009 [16] |
| 32 | 32 weeks | Spontaneous vaginal delivery | Alive | Yoruk et al., 2009 [17] |
| 28 | 37 weeks | Spontaneous vaginal delivery | Alive | Savvari et al., 2010 [18] |
| 26 | 37 weeks | Spontaneous vaginal delivery | Dead | Tazi et al., 2011 [19] |
| 17 | 15 weeks | Spontaneous abortion | Alive | Steininger et al., 2012 [20] |
| 16 | 16 weeks | C-section | Alive | Testa et al., 2013 [21] |
| 25 | 12 weeks | Not reported | Alive | Inácio Júnior et al., 2015 [22] |
3. DISCUSSION
Primary breast Burkitt lymphoma presented in a 32-year-old woman during the third trimester of pregnancy. However, the diagnosis was delayed until the postpartum period due to an initial misdiagnosis of “inflammatory mastitis” during pregnancy.
It is essential to maintain a high index of suspicion when a breast condition fails to respond to multiple courses of antibiotics. Early and accurate diagnosis is strongly correlated with improved outcomes. It can be achieved by integrating medical presentation, physical examination, and imaging findings, as the gold standard for diagnosis lies in histopathology and immunohistochemistry (IHC) studies [14].
The presentation of the current case was consistent with previously published works; a young female patient in a lactation period presented with a breast mass. However, she had no systemic symptoms commonly reported with the disease [6].
Notably, she had no history of immunosuppression or viral infection, both of which are recognizable risk factors for PB-BL. This underscores the presence of an unknown trigger for malignant transformation, warranting further investigations [5, 9, 10].
The physical examination revealed no skin changes or nipple retraction, aligning with other reported cases. However, though uncommon, bilateral involvement of the axillary LN was seen in the current case [15].
This case is the second reported case of PB-BL in Iraq. The first case reported in 2022 involved a 55-year-old woman who presented with a unilateral breast mass and positive axillary LN. She had a history of viral hepatitis and was undergoing treatment. Imaging revealed a 4x4.6 cm breast mass in the right breast with LN involvement. Histopathology confirmed PB-BL with diffuse B-cell lymphoma features. The patient declined chemotherapy and was managed with a modified radical mastectomy, followed by regular follow-up [2]. Other reported cases are summarized in Table 3.
Imaging is an important tool in many aspects of women's health; in the presented case, it plays a valuable role in establishing the diagnosis and excluding other potential causes [23-26].
While lactational mastitis is commonly seen in breastfeeding moms, PB-BL lacks key features; unlike mastitis, PB-BL lacks abscess formation. Additionally, it shows a reticular appearance and increased blood flow [4, 13].
Other differential diagnoses include other breast cancers, which typically present as an irregular hypoechoic mass that shows a length/width ratio of more than one, owing to its infiltrative deep nature, exhibiting distinct imaging characteristics [27].
Additionally, breast cancers often exhibit a surrounding echogenic ring, microcalcifications, and an enhanced post-echoing shadow [28]. Finally, PB-BL exhibits internal blood flow signals, a key feature that differentiates it from cystic breast lesions lacking vascularity [29].
Histologically, PB-BL exhibits diffuse lymphoid cell infiltration and hypoechoic nodules with reticular fibrous structures. Microscopically, the tumor exhibits a characteristic “starry sky” appearance, resulting from high proliferation and an extensive apoptosis rate among lymphoma cells [30].
An immunohistochemistry study is crucial in differentiating Burkitt lymphoma from other types, such as diffuse large B-cell lymphoma. The former has CD10 positivity, c-MYC overexpression, and a high Ki-67 index, leading to a characteristic starry sky morphology. While diffuse large B-cell lymphoma has a more variable Ki-67 index, ranging from 40% to 90%, it is more likely to have a BCL2 or BCL6 rearrangement than the MYC rearrangement [31].
Mark et al. discussed four independent predictors for reduced survival among cases receiving chemotherapy; these included patient age ≥ 40 years, central nervous system involvement, serum lactic acid dehydrogenase three times above the normal, and finally, Eastern Cooperative Oncology Group (ECOG) performance ≥ 2. The patients showed some degree of impairment, limiting daily activity [14].
Due to PB-BL's short doubling time, it needs aggressive therapy. While some cases achieve remission, others suffer from cytotoxic side effects, which may be fatal. Early diagnosis and intervention are the key to better outcomes. High-grade tumors are managed by intensive chemotherapy with an adjusted EPOCH-R regimen. The role of surgery, mastectomy, is preserved for rare, refractory cases [6].
A multidisciplinary approach is essential in managing such complex and emotionally taxing cases. Receiving a cancer diagnosis during pregnancy or in the postpartum period has profound emotional and psychological implications for any mother [32, 33].
The current case experienced significant emotional distress, not only due to concerns about her health, but also regarding her newborn's well-being. These challenges were further compounded by the additional challenges imposed by the treatment alongside infant care responsibilities [34, 35].
These factors underscore the critical need for integrated, holistic psychology and social support in addressing such complex cases. It is worth noting that AI (artificial intelligence) has shown optimistic results in enhancing breast cancer detection, particularly through imaging modalities, such as mammography, ultrasound, and MRI [36].
Deep learning models, especially convolutional neural networks, are currently being integrated into computer-aided diagnosis systems to spot subtle lesions and support clinical decisions. While the current progress is encouraging, further validation of the use of AI in breast cancer detection, screening, and diagnosis, is still needed [37].
The current report has discussed the presentation of a rare tumor, PB-BL; it was thoroughly documented with imaging studies and followed for 7 months post-remission. In addition, a comprehensive literature review was conducted to enhance the clinical relevance of the case. Still, one of the case report's limitations is that its findings cannot be generalized, especially with the absence of known risk factors, which raises the unresolved question about the underlying triggers of PB-BL. Additionally, no long-term outcomes have been reported, owing to the short follow-up period.
CONCLUSION
Primary breast Burkitt lymphoma is a highly aggressive tumor that primarily affects women of reproductive age during pregnancy and the postpartum period. It can mimic inflammatory mastitis, leading to delayed diagnosis, as seen in the current case, despite the absence of any risk factors.
The clinical presentation in this case was in line with a benign inflammatory process, and the strategy of empirical antibiotic therapy aligned with current guidelines. However, with the lack of clinical improvement, clinicians should have a high index of suspicion when a case fails to respond to standard medications; for that reason, imaging and biopsy were pursued. Although an earlier histopathological examination might have shortened the diagnostic interval, both were crucial for improving patient outcomes; the current case reflected a common diagnostic approach where inflammatory features could mask the malignancy.
While imaging studies can help differentiate the lesions, histopathological examination and immunohistochemistry remain the gold standards, with intensive chemotherapy as the cornerstone of treatment, ensuring the best chances of remission.
Initiating multi-agent intensive chemotherapy is linked with favorable patient outcomes, particularly when commenced during the early stages of the disease. A comprehensive, multidisciplinary approach is strongly recommended to optimize oncological management and address the obstetrical, neonatal, and psychological aspects of care, which are particularly critical for women during pregnancy and the postpartum period.
AUTHORS’ CONTRIBUTIONS
The authors contributed to this study as follows: W.N., S.A.F: Study conception and design; S.A.F, W.N: Data collection; Z.A.H, S.S.M, and S.K.A: Analysis and interpretation of results; W.N: Drafting of the manuscript;. All authors have read and agreed to the final version of the manuscript.
LIST OF ABBREVIATIONS
| PB-BL | = Primary breast Burkitt lymphoma |
| LN | = Lymph nodes |
| IHC | = Immunohistochemistry |
| ECOG | = Eastern Cooperative Oncology Group |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The ethical committee of Mustansiriyah Medical College, Iraq granted case approval with IRB number 253, dated 23/2/2025.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee, and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
The patient consented to the publication of the images and the data related to her case.
AVAILABILITY OF DATA AND MATERIALS
All data supporting the findings of this article were generated and analyzed by the authors. No external datasets or repositories were used. All relevant data are fully included within the manuscript.
ACKNOWLEDGEMENTS
Declared none.


