All published articles of this journal are available on ScienceDirect.
A Cipp-based Evaluation of Integrated Antenatal Care Program in Bantul, Indonesia
Abstract
Introduction
In 2022, Bantul Regency had the highest MMR in Yogyakarta Province's Special Region, with 146.8 per 100,000 live births. An integrated antenatal care (ANC) program is essential for identifying high-risk pregnant women and lowering maternal mortality. This study aims to evaluate the integrated ANC program's implementation in the Bantul Regency.
Methods
This study used a descriptive approach with CIPP model evaluation to assess program implementation in context (guidelines and SOPs), input (resources, funding, and infrastructure), process (implementation of ANC standards and obstacles), and product (ANC implementation coverage). We interviewed 18 program managers—17 PHCs and 1 district health office—using questionnaires and observation checklists in February 2024.
Results
Most study participants were doctors with undergraduate or professional degrees (72.22%). ANC guidelines and SOPs were available in all PHCs, however 29.41% lacked psychologists to provide psychological care. The lowest coverage was found in pregnancy tests, iron supplementation, and delivery counseling. The primary challenges highlighted were lack human resources (40.00%), longer integrated ANC times (20.00%), and data entry problems (10.00%).
Discussion
In Bantul Regency, integrated ANC coverage exceeds the requirements, but psychological care, pregnancy testing, iron supplementation, and delivery counseling are inadequate. Due to the absence of psychologists at some PHCs, human resources and service delivery must be prioritized to enhance maternal health outcomes, especially in high-risk populations.
Conclusion
The integrated ANC program in Bantul Regency meets implementation standards, but requires enhanced monitoring, targeted human resources, and service enhancements for low coverage. Enhanced worker capacity, service coverage, and program evaluation may improve maternal health.
1. INTRODUCTION
High Maternal Mortality Rates (MMR) in several regions indicate unequal access to quality health services. In 2017, the rate of maternal death in low-income countries was 462 per 100,000 live births, while in high-income countries it was 11 per 100,000 live births [1]. The Indonesian maternal mortality rate dropped from 346 per 100,000 live births in 2010 to 305 in 2015 and is expected to drop to 183 in 2024 [2].
The maternal mortality rate is an important metric for assessing the efficacy of maternal health-improving initiatives. The Health Profile of Yogyakarta Special Region Province in 2022 reported 43 maternal deaths. Bantul Regency has the highest rate of maternal mortality in the Yogyakarta Special Region Province, with 15 cases (146.8 per 100,000 live births) [3].
Improving the quality of integrated antenatal care (ANC) is an important intervention for reducing maternal mortality. ANC significantly reduces pregnancy-related morbidity and mortality by allowing for early detection and treatment of potential complications [4]. However, hardly one-third of expectant mothers in many underdeveloped nations make the required minimum of four visits. The quality of ANC is generally assessed by visit frequency, service delivery, adequacy of information delivered, client satisfaction, and provider competency [5].
In Indonesia, public health centers offer integrated antenatal care, including maternal-child, nutrition, dental, psychiatric, and laboratory clinics. The program follows national recommendations and provides comprehensive screening, treatments, and counseling to promote maternal and fetal health [6]. The integrated ANC program's implementation in Bantul Regency has not been evaluated. This study uses the CIPP approach to assess the implementation of an integrated ANC program in Bantul Regency, with the goal of reducing maternal mortality by early diagnosis of risk factors.
2. METHODS
2.1. Study Design
A descriptive study with structured interviews and secondary data was used to evaluate the integrated ANC program in Bantul Regency. The management-based CIPP evaluation model was used to assess integrated antenatal care by assessing four main components. The context focuses on the availability of guidelines and standards related to maternal health requirements and policies. Input evaluated resources such as program managers, qualified health workers, infrastructure, equipment, and funding to ensure service readiness. The process assessed the implementation of requirements and identified barriers. Product assessed service implementation outcomes, including ANC coverage [7]. The category indicators and product achievements are calculated from each health center's achievement outcomes. ANC program managers who provided written informed consent were included in the study. Participants who were sick or unable to attend interviews were excluded from the study to ensure data quality and consistency.
2.2. Ethical Approval
This study was approved by the Faculty of Medicine, Public Health, and Nursing's Research Ethics Committee (KE/FK/0079/EC/2024) and adhered to the ethical guidelines of the Declaration of Helsinki. Permission from the District Health Office was obtained, and all participants provided written and verbal consent.
2.3. Population and Sample
This study was conducted in Bantul Regency, which has 27 health centers distributed across 17 subdistricts. Data were collected from 17 health centers, comprising each subdistrict (62.96%), and from the District Health Office (DHO) through interviews and observations with managers of the integrated ANC program. The research was conducted in January and February 2024.
For the context and input components, we interviewed program managers from 17 health facilities and the District Health Office on integrated antenatal care program guidelines, standards, managerial roles, infrastructure, and funding. We also discussed program implementation barriers in these interviews. For the process and product components, we collected data from pregnant women receiving integrated antenatal care services at 17 health centers to assess the implementation and coverage of service standards.
The required number of samples for pregnant women was calculated using OpenEpi software. A total of 444 individuals were identified using the single population proportion formula (n = [DEFFNp(1-p)]/[(d2/Z21-α/2(N-1)+p*(1-p)]). The estimate used a 95% confidence level, a 5% margin of error, a 30% prevalence of ANC service quality based on a study in Bele Gasgar District, Ethiopia [8], a design effect of 1.3, and a 10% allowance for non-response.
2.4. Data Collection and Analysis
A structured questionnaire was used to collect data for the evaluation of the integrated ANC program. Descriptive analysis was performed in Microsoft Excel and presented in tables, graphs, and narratives to highlight key findings. Calculating frequencies, percentages, and distributions of variables described resource availability, service standard implementation, and integrated ANC service coverage. Missing data were not found in this study, and therefore, a complete dataset was accessible for analysis. The quality of integrated ANC services was defined as good when a health care facility provided at least 75% of the required focused ANC service components, which included physical examinations, basic diagnostic laboratory services, medications for treatment, danger sign counseling, birth preparation, and health advice [9].
3. RESULTS
The program evaluation found that all responders (100%) were female. The largest age group was 41–50 (38.89%) and 31–40 (38.89%). The majority of respondents had a bachelor's degree or professional education (72.22%) and were doctors (72.22%), as shown in Table 1.
In context categories, we found 100% achievement. All respondents reported that integrated ANC guidelines and standards were available in both physical and digital media at each PHC and DHO. An evaluation of inputs—including human resources, funding, and infrastructure—for integrated antenatal care showed that, while all respondents confirmed 100% availability of funding and infrastructure for integrated ANC, certain facilities have a shortage of skilled health personnel. Specifically, five community health centers (29.4%) lack psychologists, which prevents them from conducting mental health assessments. PHCs are now using the World Health Organization's Self-Reporting Questionnaire 20 (SRQ-20) to screen for mental health disorders such as anxiety and depression. This tool comprises 20 yes/no questions on experiences from the last 30 days, with the answers assessed in consultation with a general practitioner.
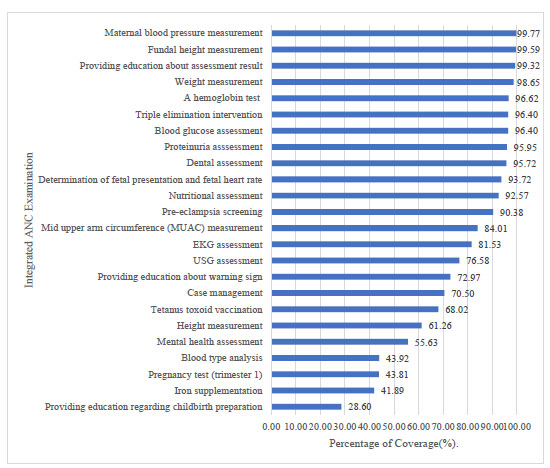
According to the process variables shown in (Fig. 1), blood pressure testing (99.77%), fundal height measurement (99.59%), and examination result counseling (99.32%) got the highest coverage. In contrast, pregnancy tests (43.81%), iron supplementation (41.89%), and delivery preparation counseling (28.60%) got the lowest coverage. This indicates areas where service delivery could be improved by highlighting gaps in preventative interventions and educational components essential for maternal and fetal health.
| Variable | Total (N=18) | Percentage (%) | |
|---|---|---|---|
| Institute | DHO | 1 | 5.56 |
| PHC | 17 | 94.44 | |
| Gender | Male | 0 | 0.00 |
| Female | 18 | 100.00 | |
| Age group (years) | 21-30 | 2 | 11.11 |
| 31-40 | 7 | 38.89 | |
| 41-50 | 7 | 38.89 | |
| 51-60 | 2 | 11.11 | |
| Education | Diploma | 2 | 11.11 |
| Undergraduate | 13 | 72.22 | |
| Master | 3 | 16.67 | |
| Occupation | Midwife | 5 | 27.78 |
| Doctor | 13 | 72.22 | |
Results of the process variable assessment.
Integrated ANC providers identified several challenges in service implementation. The main obstacles included limited human resources (40.00%), prolonged service durations (20.00%), and difficulties in entering examination result data (10.00%). These barriers may impede the efficiency and completeness of antenatal care, identifying areas that require specific adjustments for optimal service delivery.
Table S1 shows the service coverage implementation; Pleret (81.32%), Bambanglipuro (80.43%), and Piyungan (80.11%) were the three PHCs with the highest average achievement. The average accomplishment across all 17 PHCs was 79.74%, indicating a good level of service coverage throughout the area. These findings elucidate both the strengths and possible areas for enhancement, acting as a standard for improving service coverage in underperforming PHCs.
4. DISCUSSION
The assessment of Bantul Regency's integrated antenatal care (ANC) program showed that service quality was higher than the 75% criteria for good integrated ANC. This indicates that the majority of the required services, such as physical examinations, basic laboratory diagnoses, medication therapy, danger sign counseling, delivery preparation, and health advice, were successfully implemented.
In the context of components, the availability of integrated ANC guidelines and SOPs in each health center is evaluated. All respondents confirmed that each institution had these two guidelines. This integrated ANC guideline is intended to serve as a guide for providing integrated ANC to all pregnant women in Indonesia [6]. Every health center has its own SOP for integrated antenatal services based on standards. Local governments' high-quality ANC concepts are essential for integrated ANC. Prior research has shown that inadequate regulatory mechanisms or a lack of enforcement capacity are a major obstacle to quality care in public and private health facilities [10]. Therefore, guidelines and SOPs in integrated ANC are crucial for providing consistent, high-quality services, improving maternal and infant health, and increasing health service efficiency.
In the input evaluation, our findings indicate that 29.4% of public health centers (PHCs) lack a psychologist, limiting pregnant women's access to mental health assessment services at these facilities. This gap is crucial because integrated antenatal care (ANC) needs health providers to identify and manage not just nutritional deficits and obstetric difficulties, but also mental health disorders, infectious and noncommunicable diseases, to ensure a safe delivery [6]. During pregnancy and childbirth, women are vulnerable to psychological disorders. Several studies have shown that pregnant women are susceptible to stress and emotional instability [11]. Mental health issues during pregnancy can also harm a child's cognitive, emotional, and physical development [12]. Improving mental health services in ANC can increase maternal [13] and postpartum well-being [14], highlighting the need for policymakers to prioritize the allocation of mental health professionals and to integrate psychosocial support into primary health care.
The process evaluation found that pregnancy tests (43.81%), iron supplementation (41.89%), and childbirth education (28.60%) had the lowest coverage. Urine pregnancy tests are commonly used in women of reproductive age to detect pregnancy. Before further testing, urine pregnancy testing is necessary to confirm a possible pregnancy. Pregnant women with acute abdominal pain should be examined for ectopic pregnancy [15]. Our study found low coverage of urine pregnancy testing, most likely because many women accessing integrated ANC had already had this test, and certain facilities may not repeat tests until clinically required. This explanation is that repeated routine testing is frequently avoided to save costs and reduce patient burden. Standardizing ANC guidelines that specify when pregnancy tests should be repeated could increase facility consistency. Health personnel should also be trained to identify repeat testing situations while maintaining cost-effectiveness and efficiency to optimize maternal care in Indonesia.
The iron supplement tablet coverage was 41.89%. This is lower than the findings of other studies, which indicated that 94.5% of pregnant women in Ethiopia [16] and 69% in Pakistan [17] received iron supplementation. Many pregnant women experience iron deficiency anemia, which affects 15-20% of them [18]. WHO recommends daily iron and folic acid supplementation during pregnancy to reduce low birth weight, anemia, and iron deficiency. The recommended supplements are 400 mg folic acid and 30-60 mg iron, with higher doses in countries with significant public health issues, such as anaemia in pregnant women [19]. Primary care providers in Indonesia face anemia management challenges such as limited facilities, insufficiently trained staff, and barriers from pregnant women and their families [20]. Although iron supplements are often prescribed to all pregnant women, there is insufficient clarification regarding the timing and justification for hemoglobin testing [21]. Family engagement, such as reminders and support during pregnancy appointments, is critical for adherence. Addressing these systemic and cultural barriers can increase iron supplementation rates, reduce anemia prevalence, and improve maternal and child health outcomes.
This study found 28.60% coverage of integrated antenatal services for childbirth preparation explanations. This is similar to previous research conducted in Bogor City, Indonesia, which found a 23% low achievement rate [22]. Birth preparation helps pregnant women and their families anticipate delays, use necessary services during delivery, and arrive at the right facility if complications arise [23] and reduces maternal mortality [24]. In Indonesia, the rate of childbirth counseling is low, and the decision of the place of delivery is highly influenced by familial support. Husbands and close relatives are important because they are more likely to support mothers in choosing a medical facility for birth and to help them feel comfortable during the process [25]. Other research on pregnant women's classes has revealed financing limits, schedule constraints, and technical challenges. Class frequency is often limited by funding restrictions on budgets. Time constraints arise for pregnant women in the workforce, impacting attendance. Technical obstacles include limited access to educational resources and the requirement for mothers to accompany children to sessions, which delays the learning process [26]. Mitigating these obstacles is crucial to enhancing participation and the efficacy of antenatal education programs.
For the product components, the integrated ANC results in this study were 79.74%, exceeding the 75% standard for good service quality. According to the definition of good quality ANC, a health service facility must provide 75% of the required services, such as physical exams, basic diagnostic laboratory services, drug therapy, danger sign information, childbirth preparation, and advice [9]. Other research found that only 4% of pregnant women received all recommended antenatal services. Standardized ANC strongly affects maternal and fetal health during pregnancy, childbirth, and postpartum [22]. Pregnancy-related health service implementation faces more than accessibility issues. Service quality must be improved, especially to meet all pregnant women's health needs [27]. Examination coverage based on the components of integrated ANC is above average, but not all examinations are completed. This needs quality improvement to meet minimum standards. Providing high-quality, evidence-based maternal health services that meet local needs and overcome new barriers is crucial [10].
5. STUDY LIMITATIONS
This study used a descriptive method, which limits its capacity to provide a comprehensive overview of the program's implementation. The absence of qualitative data limits understanding of the experiences and views of service users. To better understand implementation procedures and contextual challenges, future research should employ qualitative techniques, such as focus groups and in-depth interviews, along with quantitative approaches to explore factors related to program implementation.
CONCLUSION
The integrated ANC program in Bantul Regency is well-implemented overall, but there are still areas for improvement. This study highlights persisting gaps in Indonesia's integrated antenatal care (ANC), specifically in mental health services, iron supplementation, pregnancy testing, and delivery preparation counseling. Systemic and cultural limitations, including inadequate health professional capacity, infrastructure, financial resources, and family involvement, reduce vital service coverage. To enhance mother and child health, policymakers must allocate adequate human and financial resources, integrate psychosocial support into primary care, standardize antenatal care protocols, improve health worker training, and promote for family-centered education. Adopting these strategies may improve adherence of recommended interventions, improve facility-based births, decrease maternal anemia and psychological issues, and ensure high-quality, evidence-based care for all pregnant women in Indonesia.
AUTHORS’ CONTRIBUTIONS
S.I.I., S.A., S.P, and B.S.W: Study conception and design; S.I.I.: Data collection; S.I.I., S.A, S.P, and B.S.W: Analysis and interpretation of results; S.I.I., B.S.W: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ANC | = Antenatal Care |
| MMR | = Maternal Mortality Rate |
| PHC | = Public Health Center |
| DHO | = District Health Office |
| SOP | = Standard Operating Procedure |
| CIPP | = Context, Input, Process, Product |
| JKN | = Jaminan Kesehatan Nasional (National Health Insurance) |
| APBD | = Anggaran Pendapatan dan Belanja Daerah (Regional Government Budget) |
| SRQ-20 | = Self-Reporting Questionnaire 20 |
| WHO | = World Health Organization |
| TB | = Tuberculosis |
| STIs | = Sexually Transmitted Infections |
| HIV | = Human Immunodeficiency Virus |
| CI | = Confidence Interval |
| DEFF | = Design Effect |
| MCH | = Maternal and Child Health |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the Research Ethics Committee of the Faculty of Medicine, Public Health, and Nursing at Universitas Gadjah Mada, Indonesia (KE/FK/0079/EC/2024).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
All participants provided verbal and written informed consent and were told that their participation was completely voluntary.
AVAILABILITY OF DATA AND MATERIAL
The data supporting the article's findings can be accessed in the Zenodo Repository at https://doi.org/ 10.5281/zenodo.17402784.
FUNDING
This research is funded by a research grant from the Faculty of Medicine, Public Health, and Nursing at Gadjah Mada University, Indonesia (1471/UN1/FKKMK/PPKE/ PT/2024) and Indonesia Endowment Fund for Education (LPDP) (Grant Number: 202207110810024). The funders had no role in the study design, data collection, analysis, publication decision, or manuscript preparation.
ACKNOWLEDGEMENTS
We appreciate all program staff in PHCs and DHO of Bantul District for their support of this study.


